Volume 9, Issue 1 (3-2021)
Jorjani Biomed J 2021, 9(1): 69-81 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
kazeminejad E, Naghashpour N. Considerations for Dental Care and Preventive Measures for COVID-19 Pandemic. Jorjani Biomed J 2021; 9 (1) :69-81
URL: http://goums.ac.ir/jorjanijournal/article-1-800-en.html
URL: http://goums.ac.ir/jorjanijournal/article-1-800-en.html
1- Dental Research Center, Golestan University of Medical Sciences, Gorgan, Iran , dr.kazeminejad@goums.ac.ir
2- Iranian Dental Association, Golestan Branch, Gorgan, Iran
2- Iranian Dental Association, Golestan Branch, Gorgan, Iran
Full-Text [PDF 695 kb]
(2078 Downloads)
| Abstract (HTML) (9539 Views)

.png)
Figure 1. Illustration of the sequence to be followed to deal with the dental patient during the COVID19 pandemic
2- Hand hygiene:
The report on the facial-oral transmission of COVID-19 shows the importance of hand hygiene for dental practices. Appropriate hand hygiene is necessary for a dental practice, but some people do not follow this protective measure, making it a tremendous challenge for controlling infection during the COVID-19 pandemic. The great importance of hand hygiene has led to a hand hygiene guideline recommendation to reinforce the observance of handwashing procedures.
The dental health staff, in particular, should wash their hands before patient examinations, before dental procedures, after touching the patient, after touching the non-disinfected environment and equipment, and after touching the oral mucosa, damaged skin or wound,
Hand hygiene is performed in two ways: either with water and soap or with alcohol-based solutions, both for 20 seconds (25).
3- Personal protective measures:
Aerosols, small and tiny particles produced by most dental procedures, can stay suspended in the air for a long time (35, 36), capable of carrying or transferring different substances such as blood, cells, restorative material particles microorganisms. Therefore, using self-protective measures like protective goggles, scrubs, face masks, face shields, protective outwear, such as a gown, and gloves are strongly recommended (37, 38).
Three levels of protective measures for spread prevention in dental professionals are suggested:
I) legal protection (primary protection):
Wearing a disposable working cap, disposable surgical mask, working clothes (scrub), protective goggles, face shield, and disposable latex or nitrile gloves.
II) advanced protection (secondary protection):
Wearing a disposable working cap, disposable surgical mask, working clothes (white coat), protective goggles, face shield, disposable latex gloves, and disposable isolation clothing or surgical clothes (gown).
III) Strengthened protection (tertiary protection):
In case of an inevitable dental treatment of a COVID-19 patient, special protective outwear is required. Working clothes (white coat) with extra disposable protective clothing outside should wear. Also, disposable cap, protective goggles, disposable surgical mask, face shield, disposable latex gloves, and impermeable shoe cover should be worn (20).
4- Mouth rinse before dental procedures:
The oral cavity is directly associated with inhalation and expelling of ambient particles during many dental procedures. Some new generations of mouth rinses include ingredients that prevent the transmission of the COVID-19 virus from the oral cavity (20, 39).
Effective ingredients that could be applied in therapeutic mouth rinses incudes:
One of the broad spectrum acting of antiseptic compounds is Chlorhexidine (CHX) 2%, which is widely used in general dentistry but may not be effective against coronaviruses (39, 40).
The 2019-nCoV is very sensitive to oxidation; therefore, using a mouth wash solution or a mouth rinse containing hydrogen peroxide 1%, povidone-iodine 0.2%, and cethyl pyridinium 0.5%- 0.1% is recommended against the influenza virus (28, 41, 42). (Table 3)
Table 3. Active ingredient concentration (W/V) of various mouthwash against SARS-Cov 2

The outbreak of the new coronavirus has led to the covid-19 pandemic, which have necessitated serious consideration in all aspects of social life as well as in the indoor dental management protocols. Paying attention to the principles of infection control in a pandemic, based on knowledge of disease transmission, considerations and appropriate discipline in performing dental procedures is of great importance.
Full-Text: (1239 Views)
Highlights
The outbreak of the new coronavirus has led to the covid-19 pandemic, which have necessitated serious consideration in all aspects of social life as well as in the indoor dental management protocols. Paying attention to the principles of infection control in a pandemic, based on knowledge of disease transmission, considerations and appropriate discipline in performing dental procedures is of great importance.
The outbreak of the new coronavirus has led to the covid-19 pandemic, which have necessitated serious consideration in all aspects of social life as well as in the indoor dental management protocols. Paying attention to the principles of infection control in a pandemic, based on knowledge of disease transmission, considerations and appropriate discipline in performing dental procedures is of great importance.
Introduction
Chinese virologists in Wuhan discovered a new virus belonging to the coronavirus family in December 2019. The virus was named SARS-CoV-2 and is a causative agent of COVID-19 disease, which can cause severe acute respiratory syndrome leading to many illnesses and death globally, and has thus become a pandemic. However, most people infected with this virus have had mild to moderate respiratory manifestations. Still, older people and those with chronic medical problems like obesity, diabetes, cardiovascular disease, chronic respiratory disease, patients receiving chemotherapy, etc., have severe manifestations with poor outcomes. Since there is no curative medicine and yet there is not complete performing vaccination to prevent the disease, understanding preventive measures is the best way to prevent the transmission of COVID-19 disease. Expelled droplets through coughing, sneezing, and, to some extent, speaking and touching surfaces contaminated with these infectious droplets could infect people with the SARS-CoV-2 virus. Health care providers are on the front line of the coronavirus pandemic and, therefore, could be easily affected. Dental procedures produce aerosols and spreading saliva droplets. These contents may be inhaled or come into contact with skin or mucous membranes or lodge on clinical surfaces and equipment and infect the dental team (1). Accordingly, having knowledge and information about the preventive measures is vital in reducing the likelihood of transmission among the dental teams and their patients. COVID-19 has caused different responses, and symptoms worldwide, which has complicated the health care system's problem, so homogeneous and global cooperation is required to deal with this pandemic (1, 2). This evidence-based study tries to a better understanding of COVID-19 and its infection control protocols for dental professions and their practice areas.
Infection control protocols address ways to prevent the spread of disease and protect dental professions and patients during pandemics. Doing practices according to these guidelines minimize the risk of infection and could help diminish the pandemic in the long term.
The primary and most crucial transmission mode for COVID-19 is through close physical contact from person-to-person via mucus secretion of patients' mouth, nose, or eyes or directly by inhalation of droplets aerosols. Droplet transmission occurs when a person is in close contact (within 1.5 meters) with someone who has respiratory symptoms (coughing, sneezing). Both symptomatic and asymptomatic patients may be a significant source of SARS-Cov 2 transmission (3).
Based on data from lab studies on COVID-19 and similar respiratory diseases, a person can get COVID-19 by touching a surface or object contaminated with the virus and then touching one's mouth, nose, or, in some rare cases, eyes. However, these are not the primary ways through which the infection could spread (4). COVID-19 likely spreads by an airborne route through aerosols produced during medical procedures (5). Airborne transmission as a form of aerosols or fomite is different from droplet transmission. It refers to the presence of viruses within droplet nuclei, which are generally considered particles < 5 µm in diameter that can remain in the air for an extended period and transmitted to others over distances higher than 1 meter. In the context of COVID-19, the airborne transmission may be possible in specific circumstances and settings in which procedures or supportive treatments that generate aerosols are performed (6, 7).
The incubation period of COVID-19 may vary from 1 to 14 days, and it reported that an asymptomatic patient could spread the virus (8-10). On a virus culture media, live viruses were shown in salivary content of infected patients by To et al. (6).
Dentists and their patients are always at risk of infections by bacteria and viruses present in the oral cavity and respiratory tract, and COVID-19 disease is an excellent threat for dentists due to face-to-face exposure to saliva, blood, and other body fluids. The risk may be increase by using sharp instruments, and pathogenic microorganisms can also be suspended in the air for an extended period that may be inhaled by dental professions (11). When people cough, sneeze or even speak at a close distance, they may propel small liquids droplets and spray aerosols from their nose or mouth, which may contain the virus and, consequently, infect the dental professions. For these reasons, environmental risk assessments, despite putting some restrictions on dental practice, could give us a better understanding of each level of dental procedures (12-15).
The present article aims marking essential needs and considerations for necessary oral health services to protect patients and the staffs working indoor private or public health centers in the outbreak of COVID-19.
Airborne spread
Many studies have proved the airborne spread of the novel coronavirus (16-18). The majority of dental procedures could produce aerosol and droplets likely to contain the coronavirus (16, 19). The large saliva and even blood containing droplets and aerosols generated by dental practices is the most important concern in dental clinics and hospitals in the spread of COVID-19 (13).
Besides the patient coughing or sneezing, some of the dental instruments like high-speed hand-pieces run by force of high-speed air, which rotates the turbine and spray water in the patient's oral cavity, could worsen the conditions. This situation can produce many aerosols and droplets mixed with saliva and even blood of the infected patients. These particles have a proper size to stay in the air for a long time enough before they settle down on environmental surfaces so they can enter the respiratory tracts of the dental staff or patients (20).
Contact spread
Frequent direct and indirect exposure of dental professionals to patients' fluids, materials, and contaminated dental instruments and environmental surfaces are the possible routes for spreading the virus (13). For these reasons, the most effective and practical strategies have to applied in infection control procedures in the daily practices of the dental offices.
Contaminated surface spread
Various coronavirus family strains can persist on surfaces like metal, glass, plastic, etc., and remain active for 4 hours up to a few days (11, 21). Such contaminated surfaces are a potential source of the spread of this virus. It has shown that H.Cov remains infectious for 2 hours up to 9 days at room temperature and can persist more in higher humidity (>50%) compared to lower ones (<30%) level (20). Thus, keeping dental offices clean and dry would decrease the persistence of SARS-CoV2. (Table 1)
However, several studies have questioned the amount of viral load transmitted from the surface to the host, and in fact do not consider surface transfer to be as effective as airborne transmission (22-24).
Chinese virologists in Wuhan discovered a new virus belonging to the coronavirus family in December 2019. The virus was named SARS-CoV-2 and is a causative agent of COVID-19 disease, which can cause severe acute respiratory syndrome leading to many illnesses and death globally, and has thus become a pandemic. However, most people infected with this virus have had mild to moderate respiratory manifestations. Still, older people and those with chronic medical problems like obesity, diabetes, cardiovascular disease, chronic respiratory disease, patients receiving chemotherapy, etc., have severe manifestations with poor outcomes. Since there is no curative medicine and yet there is not complete performing vaccination to prevent the disease, understanding preventive measures is the best way to prevent the transmission of COVID-19 disease. Expelled droplets through coughing, sneezing, and, to some extent, speaking and touching surfaces contaminated with these infectious droplets could infect people with the SARS-CoV-2 virus. Health care providers are on the front line of the coronavirus pandemic and, therefore, could be easily affected. Dental procedures produce aerosols and spreading saliva droplets. These contents may be inhaled or come into contact with skin or mucous membranes or lodge on clinical surfaces and equipment and infect the dental team (1). Accordingly, having knowledge and information about the preventive measures is vital in reducing the likelihood of transmission among the dental teams and their patients. COVID-19 has caused different responses, and symptoms worldwide, which has complicated the health care system's problem, so homogeneous and global cooperation is required to deal with this pandemic (1, 2). This evidence-based study tries to a better understanding of COVID-19 and its infection control protocols for dental professions and their practice areas.
Infection control protocols address ways to prevent the spread of disease and protect dental professions and patients during pandemics. Doing practices according to these guidelines minimize the risk of infection and could help diminish the pandemic in the long term.
The primary and most crucial transmission mode for COVID-19 is through close physical contact from person-to-person via mucus secretion of patients' mouth, nose, or eyes or directly by inhalation of droplets aerosols. Droplet transmission occurs when a person is in close contact (within 1.5 meters) with someone who has respiratory symptoms (coughing, sneezing). Both symptomatic and asymptomatic patients may be a significant source of SARS-Cov 2 transmission (3).
Based on data from lab studies on COVID-19 and similar respiratory diseases, a person can get COVID-19 by touching a surface or object contaminated with the virus and then touching one's mouth, nose, or, in some rare cases, eyes. However, these are not the primary ways through which the infection could spread (4). COVID-19 likely spreads by an airborne route through aerosols produced during medical procedures (5). Airborne transmission as a form of aerosols or fomite is different from droplet transmission. It refers to the presence of viruses within droplet nuclei, which are generally considered particles < 5 µm in diameter that can remain in the air for an extended period and transmitted to others over distances higher than 1 meter. In the context of COVID-19, the airborne transmission may be possible in specific circumstances and settings in which procedures or supportive treatments that generate aerosols are performed (6, 7).
The incubation period of COVID-19 may vary from 1 to 14 days, and it reported that an asymptomatic patient could spread the virus (8-10). On a virus culture media, live viruses were shown in salivary content of infected patients by To et al. (6).
Dentists and their patients are always at risk of infections by bacteria and viruses present in the oral cavity and respiratory tract, and COVID-19 disease is an excellent threat for dentists due to face-to-face exposure to saliva, blood, and other body fluids. The risk may be increase by using sharp instruments, and pathogenic microorganisms can also be suspended in the air for an extended period that may be inhaled by dental professions (11). When people cough, sneeze or even speak at a close distance, they may propel small liquids droplets and spray aerosols from their nose or mouth, which may contain the virus and, consequently, infect the dental professions. For these reasons, environmental risk assessments, despite putting some restrictions on dental practice, could give us a better understanding of each level of dental procedures (12-15).
The present article aims marking essential needs and considerations for necessary oral health services to protect patients and the staffs working indoor private or public health centers in the outbreak of COVID-19.
Airborne spread
Many studies have proved the airborne spread of the novel coronavirus (16-18). The majority of dental procedures could produce aerosol and droplets likely to contain the coronavirus (16, 19). The large saliva and even blood containing droplets and aerosols generated by dental practices is the most important concern in dental clinics and hospitals in the spread of COVID-19 (13).
Besides the patient coughing or sneezing, some of the dental instruments like high-speed hand-pieces run by force of high-speed air, which rotates the turbine and spray water in the patient's oral cavity, could worsen the conditions. This situation can produce many aerosols and droplets mixed with saliva and even blood of the infected patients. These particles have a proper size to stay in the air for a long time enough before they settle down on environmental surfaces so they can enter the respiratory tracts of the dental staff or patients (20).
Contact spread
Frequent direct and indirect exposure of dental professionals to patients' fluids, materials, and contaminated dental instruments and environmental surfaces are the possible routes for spreading the virus (13). For these reasons, the most effective and practical strategies have to applied in infection control procedures in the daily practices of the dental offices.
Contaminated surface spread
Various coronavirus family strains can persist on surfaces like metal, glass, plastic, etc., and remain active for 4 hours up to a few days (11, 21). Such contaminated surfaces are a potential source of the spread of this virus. It has shown that H.Cov remains infectious for 2 hours up to 9 days at room temperature and can persist more in higher humidity (>50%) compared to lower ones (<30%) level (20). Thus, keeping dental offices clean and dry would decrease the persistence of SARS-CoV2. (Table 1)
However, several studies have questioned the amount of viral load transmitted from the surface to the host, and in fact do not consider surface transfer to be as effective as airborne transmission (22-24).
Table 1. Stability of SARS-CoV2 at various conditions
| Based on lab temperature/ humidity 65% |
Based on The surfaces Temperature 22 °C / humidity 65% | Stability of SARS-Cov2 against on Disinfectants | |||
| Temperature | Survival time | Surfaces | Survival time | Disinfectant | Survival time |
| 4°C | >14 days | Paper / tissue paper | 3 hours | Diluted bleach (1: 49) |
5 mins |
| 22°C | 14 days | Wood / cloth | 2 days | Diluted bleach (1: 49) |
5 mins |
| 37°C | 2 days | glass | 4 days | Hand Soap solution(1:49) | 15 mins |
| 56°C |
30 mins | banknote | 4 days | Ethanol 70% | 5 mins |
| 70°C | 5 mins | Stainless steel / plastic | 7 days | Povidone-iodine 7.5% | 5 mins |
| Mask, inner layer | 7 days | Chloroxylenol 0.05% | 5 mins | ||
| Mask, outer layer | >7 days | Chlorhexidine 0.05% |
5 mins | ||
| Benzalkonium chloride 0.1% | 5 mins | ||||
Note: mins=minutes.
Infection controls for dental practice:
Since it is has been proved that aerosols and droplets are the main routes of spread for the 2019-nCov, taking the following steps is essential to ensure doing safe dental practices:
1- Patient evaluation:
The dental clinic should not accept patients in the acute febrile phase of the disease for any dental procedures. If dental professionals identify an infected person, the case should not be treated and should be quarantined and reported to the case infection control department immediately (25). The waiting room of the dental practice or center should be sufficiently ventilated. Before the patient's entry to the dental chair-side, the patient should wear a surgical or face mask and use disinfectant gel. Also, the patient temperature should measure with a sterile or contact-free forehead thermometer, and the following questions should ask:
A) Do you have or experienced fever over the past two weeks?
B) Have you experienced any respiratory problems like a cough or difficult breathing during the past two weeks?
C) Have you had any contact with documented COVID-19 patients?
D) Have you had any contact with confirmed COVID-19 patients during the past two weeks?
E) Have you recently participated in any gathering, meeting, or close contact with unacquainted people?
If the answer is "yes" to any of the above questions, and the patient's body temperature is above 37.5°C, the dentist should defer treatment for the next 14 days (26-28). (Figure 1)
Since it is has been proved that aerosols and droplets are the main routes of spread for the 2019-nCov, taking the following steps is essential to ensure doing safe dental practices:
1- Patient evaluation:
The dental clinic should not accept patients in the acute febrile phase of the disease for any dental procedures. If dental professionals identify an infected person, the case should not be treated and should be quarantined and reported to the case infection control department immediately (25). The waiting room of the dental practice or center should be sufficiently ventilated. Before the patient's entry to the dental chair-side, the patient should wear a surgical or face mask and use disinfectant gel. Also, the patient temperature should measure with a sterile or contact-free forehead thermometer, and the following questions should ask:
A) Do you have or experienced fever over the past two weeks?
B) Have you experienced any respiratory problems like a cough or difficult breathing during the past two weeks?
C) Have you had any contact with documented COVID-19 patients?
D) Have you had any contact with confirmed COVID-19 patients during the past two weeks?
E) Have you recently participated in any gathering, meeting, or close contact with unacquainted people?
If the answer is "yes" to any of the above questions, and the patient's body temperature is above 37.5°C, the dentist should defer treatment for the next 14 days (26-28). (Figure 1)
.png)
Figure 1. Illustration of the sequence to be followed to deal with the dental patient during the COVID19 pandemic
A patient with the diagnosed symptoms may have a positive nasopharyngeal swab on reverse transcriptase-polymerase chain reaction (RP- PCR) test for the virus genome sequences. It is also recommended that obtaining at least two negative PCR tests repeatedly after resolving the symptoms must be needed to confirm covid-19 recovery. (29-31)
Unfortunately, there is a numerous false-negative result for PCR test based on the sampling procedures and the technical errors. (32)
Moreover, the antibodies against the SARS-COV-2 antigens could detect in the serum of the covid-19 patients. The seroconversion usually appears after three weeks of the symptoms' onset. The time for this seroconversion is named the window period. (33, 34)
Interpretation of IgG and IgM seroconversion change concerning considering PCR test results may help evaluate the patients with covid-19 (31). (Table 2)
Unfortunately, there is a numerous false-negative result for PCR test based on the sampling procedures and the technical errors. (32)
Moreover, the antibodies against the SARS-COV-2 antigens could detect in the serum of the covid-19 patients. The seroconversion usually appears after three weeks of the symptoms' onset. The time for this seroconversion is named the window period. (33, 34)
Interpretation of IgG and IgM seroconversion change concerning considering PCR test results may help evaluate the patients with covid-19 (31). (Table 2)
Table 2. Interpretation of the PCR, IgG and IgM results
| Test Result | Clinical findings | ||
| PCR | IgM | IgG | |
| + | - | - | The patient may be in the early phase of the window period |
| + | + | - | The patient may be in the early phase of SARS-COV-2 infection |
| + | + | + | The patient involved with the active phase of the infection |
| + | - | + | The patient may be in the late stage or recurrent situation of infection |
| - | + | - | The patient may be in the early phase of the infection or false-negative result of the PCR |
| - | - | + | The patient may have had recovered from a past infection |
| - | + | + | The patient may be in a recovery phase, or a false-negative result of the PCR |
2- Hand hygiene:
The report on the facial-oral transmission of COVID-19 shows the importance of hand hygiene for dental practices. Appropriate hand hygiene is necessary for a dental practice, but some people do not follow this protective measure, making it a tremendous challenge for controlling infection during the COVID-19 pandemic. The great importance of hand hygiene has led to a hand hygiene guideline recommendation to reinforce the observance of handwashing procedures.
The dental health staff, in particular, should wash their hands before patient examinations, before dental procedures, after touching the patient, after touching the non-disinfected environment and equipment, and after touching the oral mucosa, damaged skin or wound,
Hand hygiene is performed in two ways: either with water and soap or with alcohol-based solutions, both for 20 seconds (25).
3- Personal protective measures:
Aerosols, small and tiny particles produced by most dental procedures, can stay suspended in the air for a long time (35, 36), capable of carrying or transferring different substances such as blood, cells, restorative material particles microorganisms. Therefore, using self-protective measures like protective goggles, scrubs, face masks, face shields, protective outwear, such as a gown, and gloves are strongly recommended (37, 38).
Three levels of protective measures for spread prevention in dental professionals are suggested:
I) legal protection (primary protection):
Wearing a disposable working cap, disposable surgical mask, working clothes (scrub), protective goggles, face shield, and disposable latex or nitrile gloves.
II) advanced protection (secondary protection):
Wearing a disposable working cap, disposable surgical mask, working clothes (white coat), protective goggles, face shield, disposable latex gloves, and disposable isolation clothing or surgical clothes (gown).
III) Strengthened protection (tertiary protection):
In case of an inevitable dental treatment of a COVID-19 patient, special protective outwear is required. Working clothes (white coat) with extra disposable protective clothing outside should wear. Also, disposable cap, protective goggles, disposable surgical mask, face shield, disposable latex gloves, and impermeable shoe cover should be worn (20).
4- Mouth rinse before dental procedures:
The oral cavity is directly associated with inhalation and expelling of ambient particles during many dental procedures. Some new generations of mouth rinses include ingredients that prevent the transmission of the COVID-19 virus from the oral cavity (20, 39).
Effective ingredients that could be applied in therapeutic mouth rinses incudes:
One of the broad spectrum acting of antiseptic compounds is Chlorhexidine (CHX) 2%, which is widely used in general dentistry but may not be effective against coronaviruses (39, 40).
The 2019-nCoV is very sensitive to oxidation; therefore, using a mouth wash solution or a mouth rinse containing hydrogen peroxide 1%, povidone-iodine 0.2%, and cethyl pyridinium 0.5%- 0.1% is recommended against the influenza virus (28, 41, 42). (Table 3)
Table 3. Active ingredient concentration (W/V) of various mouthwash against SARS-Cov 2
| Mouthwash (active ingredient) | Content % | Rinsing time | Evidence-based approval |
| Hydrogen peroxide | 1% | 1 min | yes |
| Povidone-iodine | 0. 2% | 1min | yes |
| Cetylpyridinium- chloride | 0.5% | 1min | yes |
| chlorhexidine | 0.2% | 1min | Not yet |
Note: W/V=weight per volume.
5- Rubber dam isolation:
High-speed dental handpieces or ultrasonic devices may produce a tremendous volume of saliva and bloody contaminated aerosols and droplets, but using rubber dam can significantly decrease these contaminated particles. Even when the rubber dam is applied, a high-volume evacuator (HVE) is also recommended. In this situation, the four-handed technique is usually practiced. If the rubber dam technique is not possible in some cases, some material and manual devices, such as Carisolve and hand scaler, are proposed for caries removal and periodontal scaling to minimize aerosols generation (20, 28, 43).
6- Anti-retraction handpiece:
The debris and fluids may be aspirated and expelled during the dental procedures using a high-speed dental handpiece without anti-retraction valves. Microorganisms like bacteria and viruses can contaminate the air and water tubes within the dental units and potentially cause cross-infection. Studies have shown that using anti-refractive high-speed handpieces can dramatically reduce the back flue of oral microorganisms (20, 43).
7- Disinfection of the clinic settings:
Human-to-human transmission happens within 2-14 days after exposure to the spreading droplets or aerosols in the air by coughing, sneezing, and also touching the contaminated hands or surfaces. Virologists have shown that the virus can survive up to 3 hours in the air in tiny droplets (11). When these droplets land on various surfaces, they behave differently depending on the type of surfaces. It remains alive on plastic for about 24 hours, on materials like aluminum for about 8 hours, on copper for only 4 hours, and on glass or wooden surfaces for about 4 days. Moreover, the coronavirus can be eradicated within one minute by disinfecting surfaces with alcohol 70%, hydrogen peroxide 0.5%, or bleach dilution containing 0.1% sodium hypochlorite (11, 44).
In waiting rooms and reception areas of urgent dental care centers, a two-meter social distancing rule between the patients' needs to observe. The whole medical environment should be kept clean and tidy, so all non-essential items like toys, books, magazines should remove. All urgent dental care centers have to follow standard infection control procedures and transmission-based protocols to diminish the likelihood of the spread of the COVID-19 virus. Careful cleaning and disinfecting of all the working surfaces after treating each patient is recommended. Cleaning and disinfection should be done with a disinfectant that contains a sodium hypochlorite solution of 0.1%-0.5% of active chlorine. Doing this could eradicate the virus after a minute of contact with ordinary disinfectants like household bleach (11, 44).
8- Management of airborne and, aerosol infection transmission:
Many dental professionals are looking for ways to reduce aerosols and splatter in dentistry and provide clean air quality in their dental offices.
The best idea to achieve a clean air quality is to construct a simplified airborne infection rooms (AIIRs) with negative pressure. We can install single ventilation unite into an ordinary patient room. The negative pressure is maintained by a ventilation system that takes more air out of the room than is allowed to enter. In contrast, the purification system has purified the air by a high-efficiency particular air (HEPA) filter. In this way, dental professions can remove the virus that might be in the air from the dental procedure room (45, 46).
The H14 class of HEPA filter can remove more than 99.975% of airborne particles down to 0.3 microns in size (47). This means that only three can be permitted to escape for every 10000 particles that pass through the filter.
To prevent the transmission of COVID-19 disease, using high-suction devices, such as high volume evacuators (HVE), and having a great air conditioning system with good HEPA or equivalent filters is another way to reduce a large number of human pathogens in dental centers. To achieve this purpose, a few products and disciplines must be should be used to help minimize the number of aerosols and reduce the clinicians' exposure to droplets containing SARS- Cov2 viruses. The dental team may believe that they are protected from airborne contaminations through a building's heating, ventilation, and air conditioning (HVAC) system. Service your HVAC system to ensure that it works appropriately and functionally. It is also essential to use high-quality filters and replace them regularly and properly (45, 48). As an addition, the ventilation supply unit installs to recirculate and exchange the large air volume from the patient room. It is essential to maintain the ventilation of the dental office's contaminated air ≥12 times per hour (45, 46).
Disinfection of surfaces and partly contaminated by SARS- Cov2 virus and aerosols can achieve by using ultraviolet light. There are three UV-light classes: vacuum UV, far UV, UV-C, UV-B, and UV-A (49).
UV-A and UV-B light cause sunburns, premature skin aging and may, ultimately, lead to skin cancer. Vacuum UV, far UV, and UV-C light have the most energy of all three types, respectively. But it, fortunately, does not reach the earth because of the absorbent of the atmosphere. There is human-made UV-C light, too, which exist in UV light sanitizers that companies claim kill the coronavirus.
UV-C light can destroy coronavirus and microbes by breaking down the genetic material, either DNA or RNA structure of them. It produces some photo dimers and incorporates them into the viruses' genomic material as a Trojan (50). As a result, the virus either dies or loses its capability of replicating. That means the ultraviolet rays must directly strike the virus, and all of the surfaces and equipment must be directly exposed to UV light for disinfection. Thus, any part that falls within a shadow might still carry active coronavirus. So two or three-five-minute rounds of ultraviolet radiation leave pathogens too damaged to function.
Moreover, for gaining the right and optimum results in disinfection, the UV light's exact fluency dose should be calculate based on distance from objects, irradiation power, and some technical variables by the expert. Therefore, the specification of the UV generators may differ for this mitigation in every place (50, 51).
9- Disinfection of dental impressions:
As we know, cross-infection from microbial contaminated dental impressions is recognized. There are, therefore, some instructions to reduce the transmission between dental professionals and laboratories.
- All the impression trays should be cleaned and heat sterilized for both the patient and professionals' safety.
- The impressions need to be washed with running water or brushed altogether to cast off all the particles, blood, and saliva.
- The dental impressions, such as polysulfide, additional silicon, and alginate, should be disinfect. Accordingly, it is necessary to submerge the impressions into sodium hypochlorite 0.5% (NaOCl) for at least 10 minutes (52, 53).
- Impression will undoubtedly lead to surface changes or distortion in the case of gels, such as alginate and expansion of polyethers after 10 minutes, so spraying with a Microzid or Sodium hypochlorite solution 0.5% need to be considered (54, 55).
- We should also use a 5.25% concentration of Sodium hypochlorite with the shortest contact time of one minute (56).
- Alcohol is also contraindicated for impression disinfection due to surface changes that it could cause.
- Dental impressions should not be stored or carried without hygienic packing.
10- Management of medical waste:
Disposable protective equipment creates the medical and domestic waste that dispose as B Class of waste material in dental office or clinics which cause harm to the dental staff, the patients, and the environment (57).
It is essential that both the ordinary and medical wastes with suspected or confirmed 2019-nCoV infection need to be enclosed in two yellow biomedical waste bags, marked as an infected medical waste, sealed properly and, finally, demolished following the regular rules (58).
Conclusion
The widespread outbreak of COVID-19 is a severe threat to humans' health, well-being, and survival. The characteristics of dental treatments and the possibility of aerosol production during treatment could classify dentistry as one of the most high-risk jobs in the world. The existing knowledge of COVID-19 is currently limited, and performing vaccination, effective medicinal drugs, and possible treatments are imminent. Comprehensive research and investigations are needed to clarify COVID-19 routes of transmission, pathogenicity, and it's mechanisms, and also define potential pharmaceutical purposes. Notwithstanding these complexities, cleaning and disinfecting the hands and all work surfaces after treating patients could prevent cross-contamination. As the main guideline, the patients should consider not attending the clinic if they believe it does not have the appropriate care and protection conditions. Only urgent dental treatments need to be carried out. In conclusion, although the list of precautions could continue, the only way to beat the coronavirus crisis is "to do our part." Acknowledgment
The authors would like to express their special thanks to the Dental Research Center at Golestan University of Medical Sciences and Health Services in Gorgan, Iran.
This article wrote after receiving ethics approval from the ethics committee in Golestan University of Medical Sciences, Iran (IR.GOUMS.REC.1399.089).
Conflict of interests
There are no conflicts of interest for the authors and publication of this article.
Graphical Abstract
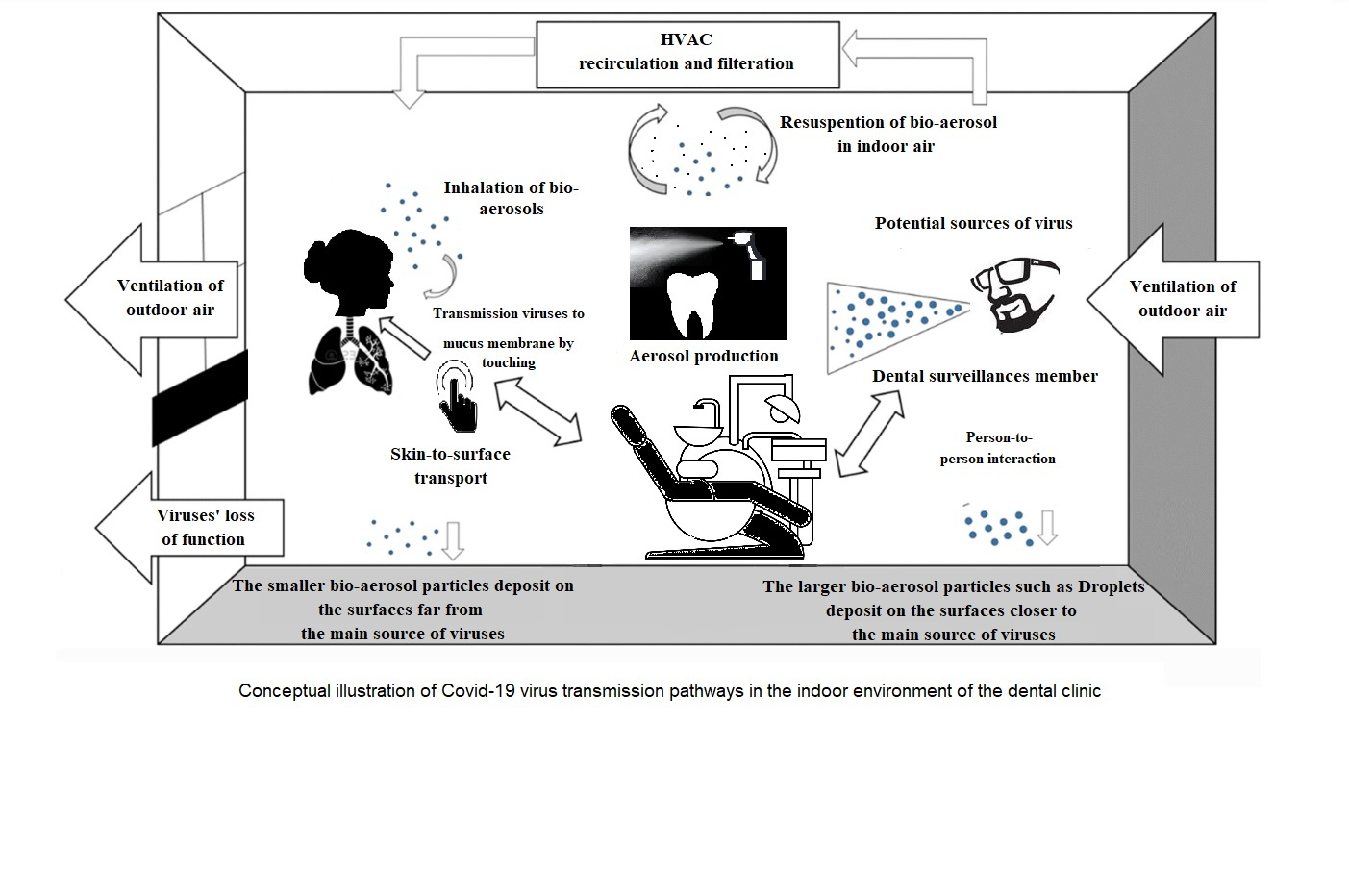
Conceptual illustration of covid-19 virus transmission pathways in the indoor environment of the dental clinic
5- Rubber dam isolation:
High-speed dental handpieces or ultrasonic devices may produce a tremendous volume of saliva and bloody contaminated aerosols and droplets, but using rubber dam can significantly decrease these contaminated particles. Even when the rubber dam is applied, a high-volume evacuator (HVE) is also recommended. In this situation, the four-handed technique is usually practiced. If the rubber dam technique is not possible in some cases, some material and manual devices, such as Carisolve and hand scaler, are proposed for caries removal and periodontal scaling to minimize aerosols generation (20, 28, 43).
6- Anti-retraction handpiece:
The debris and fluids may be aspirated and expelled during the dental procedures using a high-speed dental handpiece without anti-retraction valves. Microorganisms like bacteria and viruses can contaminate the air and water tubes within the dental units and potentially cause cross-infection. Studies have shown that using anti-refractive high-speed handpieces can dramatically reduce the back flue of oral microorganisms (20, 43).
7- Disinfection of the clinic settings:
Human-to-human transmission happens within 2-14 days after exposure to the spreading droplets or aerosols in the air by coughing, sneezing, and also touching the contaminated hands or surfaces. Virologists have shown that the virus can survive up to 3 hours in the air in tiny droplets (11). When these droplets land on various surfaces, they behave differently depending on the type of surfaces. It remains alive on plastic for about 24 hours, on materials like aluminum for about 8 hours, on copper for only 4 hours, and on glass or wooden surfaces for about 4 days. Moreover, the coronavirus can be eradicated within one minute by disinfecting surfaces with alcohol 70%, hydrogen peroxide 0.5%, or bleach dilution containing 0.1% sodium hypochlorite (11, 44).
In waiting rooms and reception areas of urgent dental care centers, a two-meter social distancing rule between the patients' needs to observe. The whole medical environment should be kept clean and tidy, so all non-essential items like toys, books, magazines should remove. All urgent dental care centers have to follow standard infection control procedures and transmission-based protocols to diminish the likelihood of the spread of the COVID-19 virus. Careful cleaning and disinfecting of all the working surfaces after treating each patient is recommended. Cleaning and disinfection should be done with a disinfectant that contains a sodium hypochlorite solution of 0.1%-0.5% of active chlorine. Doing this could eradicate the virus after a minute of contact with ordinary disinfectants like household bleach (11, 44).
8- Management of airborne and, aerosol infection transmission:
Many dental professionals are looking for ways to reduce aerosols and splatter in dentistry and provide clean air quality in their dental offices.
The best idea to achieve a clean air quality is to construct a simplified airborne infection rooms (AIIRs) with negative pressure. We can install single ventilation unite into an ordinary patient room. The negative pressure is maintained by a ventilation system that takes more air out of the room than is allowed to enter. In contrast, the purification system has purified the air by a high-efficiency particular air (HEPA) filter. In this way, dental professions can remove the virus that might be in the air from the dental procedure room (45, 46).
The H14 class of HEPA filter can remove more than 99.975% of airborne particles down to 0.3 microns in size (47). This means that only three can be permitted to escape for every 10000 particles that pass through the filter.
To prevent the transmission of COVID-19 disease, using high-suction devices, such as high volume evacuators (HVE), and having a great air conditioning system with good HEPA or equivalent filters is another way to reduce a large number of human pathogens in dental centers. To achieve this purpose, a few products and disciplines must be should be used to help minimize the number of aerosols and reduce the clinicians' exposure to droplets containing SARS- Cov2 viruses. The dental team may believe that they are protected from airborne contaminations through a building's heating, ventilation, and air conditioning (HVAC) system. Service your HVAC system to ensure that it works appropriately and functionally. It is also essential to use high-quality filters and replace them regularly and properly (45, 48). As an addition, the ventilation supply unit installs to recirculate and exchange the large air volume from the patient room. It is essential to maintain the ventilation of the dental office's contaminated air ≥12 times per hour (45, 46).
Disinfection of surfaces and partly contaminated by SARS- Cov2 virus and aerosols can achieve by using ultraviolet light. There are three UV-light classes: vacuum UV, far UV, UV-C, UV-B, and UV-A (49).
UV-A and UV-B light cause sunburns, premature skin aging and may, ultimately, lead to skin cancer. Vacuum UV, far UV, and UV-C light have the most energy of all three types, respectively. But it, fortunately, does not reach the earth because of the absorbent of the atmosphere. There is human-made UV-C light, too, which exist in UV light sanitizers that companies claim kill the coronavirus.
UV-C light can destroy coronavirus and microbes by breaking down the genetic material, either DNA or RNA structure of them. It produces some photo dimers and incorporates them into the viruses' genomic material as a Trojan (50). As a result, the virus either dies or loses its capability of replicating. That means the ultraviolet rays must directly strike the virus, and all of the surfaces and equipment must be directly exposed to UV light for disinfection. Thus, any part that falls within a shadow might still carry active coronavirus. So two or three-five-minute rounds of ultraviolet radiation leave pathogens too damaged to function.
Moreover, for gaining the right and optimum results in disinfection, the UV light's exact fluency dose should be calculate based on distance from objects, irradiation power, and some technical variables by the expert. Therefore, the specification of the UV generators may differ for this mitigation in every place (50, 51).
9- Disinfection of dental impressions:
As we know, cross-infection from microbial contaminated dental impressions is recognized. There are, therefore, some instructions to reduce the transmission between dental professionals and laboratories.
- All the impression trays should be cleaned and heat sterilized for both the patient and professionals' safety.
- The impressions need to be washed with running water or brushed altogether to cast off all the particles, blood, and saliva.
- The dental impressions, such as polysulfide, additional silicon, and alginate, should be disinfect. Accordingly, it is necessary to submerge the impressions into sodium hypochlorite 0.5% (NaOCl) for at least 10 minutes (52, 53).
- Impression will undoubtedly lead to surface changes or distortion in the case of gels, such as alginate and expansion of polyethers after 10 minutes, so spraying with a Microzid or Sodium hypochlorite solution 0.5% need to be considered (54, 55).
- We should also use a 5.25% concentration of Sodium hypochlorite with the shortest contact time of one minute (56).
- Alcohol is also contraindicated for impression disinfection due to surface changes that it could cause.
- Dental impressions should not be stored or carried without hygienic packing.
10- Management of medical waste:
Disposable protective equipment creates the medical and domestic waste that dispose as B Class of waste material in dental office or clinics which cause harm to the dental staff, the patients, and the environment (57).
It is essential that both the ordinary and medical wastes with suspected or confirmed 2019-nCoV infection need to be enclosed in two yellow biomedical waste bags, marked as an infected medical waste, sealed properly and, finally, demolished following the regular rules (58).
Conclusion
The widespread outbreak of COVID-19 is a severe threat to humans' health, well-being, and survival. The characteristics of dental treatments and the possibility of aerosol production during treatment could classify dentistry as one of the most high-risk jobs in the world. The existing knowledge of COVID-19 is currently limited, and performing vaccination, effective medicinal drugs, and possible treatments are imminent. Comprehensive research and investigations are needed to clarify COVID-19 routes of transmission, pathogenicity, and it's mechanisms, and also define potential pharmaceutical purposes. Notwithstanding these complexities, cleaning and disinfecting the hands and all work surfaces after treating patients could prevent cross-contamination. As the main guideline, the patients should consider not attending the clinic if they believe it does not have the appropriate care and protection conditions. Only urgent dental treatments need to be carried out. In conclusion, although the list of precautions could continue, the only way to beat the coronavirus crisis is "to do our part." Acknowledgment
The authors would like to express their special thanks to the Dental Research Center at Golestan University of Medical Sciences and Health Services in Gorgan, Iran.
This article wrote after receiving ethics approval from the ethics committee in Golestan University of Medical Sciences, Iran (IR.GOUMS.REC.1399.089).
Conflict of interests
There are no conflicts of interest for the authors and publication of this article.
Graphical Abstract
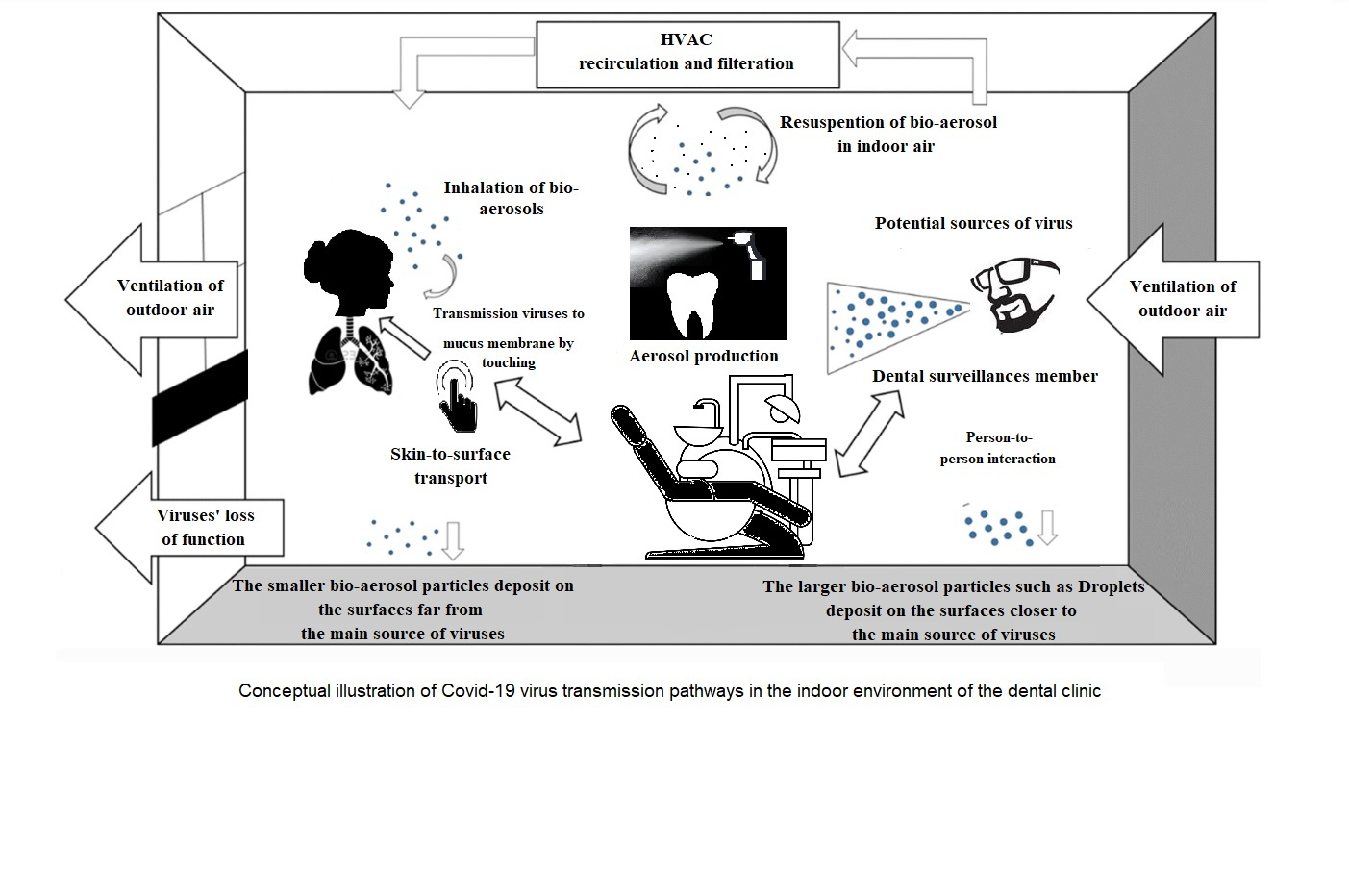
Conceptual illustration of covid-19 virus transmission pathways in the indoor environment of the dental clinic
|
Type of Article: Review Article |
Subject:
General medicine
Received: 2021/02/11 | Accepted: 2021/03/7 | Published: 2021/03/30
Received: 2021/02/11 | Accepted: 2021/03/7 | Published: 2021/03/30
References
1. Meng L, Hua F, Bian Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J Dent Res. 2020;99(5):481-7. [view at publisher] [DOI] [Google Scholar]
2. Coulthard P. Dentistry and coronavirus (COVID-19) - moral decision-making. Br Dent J. 2020;228 (7):503-505. [view at publisher] [DOI] [Google Scholar]
3. Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):e39. [view at publisher] [DOI] [Google Scholar]
4. Belser JA, Rota PA, Tumpey TM. Ocular tropism of respiratory viruses. Microbiol Mol Biol Rev. 2013;77(1):144-56. [DOI] [Google Scholar]
5. Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67(5):568-76. [view at publisher] [DOI] [Google Scholar]
6. To KK, Tsang OT, Chik-Yan Yip C, Chan KH, Wu TC, Chan JMC, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020. [view at publisher] [DOI] [Google Scholar]
7. Rodriguez-Morales AJ, MacGregor K, Kanagarajah S, Patel D, Schlagenhauf P. Going global - Travel and the 2019 novel coronavirus. Travel Med Infect Dis. 2020;33:101578. [view at publisher] [DOI] [Google Scholar]
8. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. [view at publisher] [DOI] [Google Scholar]
9. Guan W-j, Ni Z-y, Hu Y, Liang W-h, Ou C-q, He J-x, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. New England Journal of Medicine. 2020;382(18):1708-20. [view at publisher] [DOI] [Google Scholar]
10. Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020. Euro Surveill. 2020;25(5). [view at publisher] [DOI] [Google Scholar]
11. Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104(3):246-51. [view at publisher] [DOI] [Google Scholar]
12. Chen J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect. 2020;22(2):69-71. [view at publisher] [DOI] [Google Scholar]
13. Cleveland JL, Gray SK, Harte JA, Robison VA, Moorman AC, Gooch BF. Transmission of blood-borne pathogens in US dental health care settings: 2016 update. J Am Dent Assoc. 2016;147(9):729-38. [view at publisher] [DOI] [Google Scholar]
14. Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135(4):429-37. [view at publisher] [DOI] [Google Scholar]
15. Liu L, Wei Q, Alvarez X, Wang H, Du Y, Zhu H, et al. Epithelial cells lining salivary gland ducts are early target cells of severe acute respiratory syndrome coronavirus infection in the upper respiratory tracts of rhesus macaques. J Virol. 2011;85(8):4025-30. [DOI] [Google Scholar]
16. Wei J, Li Y. Airborne spread of infectious agents in the indoor environment. Am J Infect Control. 2016;44(9 Suppl):S102-8. [view at publisher] [DOI] [Google Scholar]
17. Morawska L, Cao J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environ Int. 2020;139:105730-. [view at publisher] [DOI] [Google Scholar]
18. Stern RA, Koutrakis P, Martins MAG, Lemos B, Dowd SE, Sunderland EM, et al. Characterization of hospital airborne SARS-CoV-2. Respiratory Research. 2021;22(1):73. [view at publisher] [DOI] [Google Scholar]
19. Semelka C, Ornelles D, Connell N, Parsons E, Blevins M, Ivey L, et al. Detection of Environmental Spread of SARS-CoV-2 and Associated Patient Characteristics. Open Forum Infectious Diseases. 2021. [DOI] [Google Scholar]
20. Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. International Journal of Oral Science. 2020;12(1):9. [view at publisher] [DOI] [Google Scholar]
21. Otter JA, Donskey C, Yezli S, Douthwaite S, Goldenberg SD, Weber DJ. Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. J Hosp Infect. 2016;92(3):235-50. [view at publisher] [DOI] [Google Scholar]
22. Goldman E. Exaggerated risk of transmission of COVID-19 by fomites. The Lancet Infectious Diseases. 2020;20. [view at publisher] [DOI] [Google Scholar]
23. Kraay A, Hayashi M, Berendes D, Sobolik J, Leon J, Lopman B. Risk of fomite-mediated transmission of SARS-CoV-2 in child daycares, schools, and offices: a modeling study2020 [view at publisher] [DOI] [Google Scholar]
24. Ijaz MK, Nims R, McKinney J. Indirect transmission of SARS-CoV-2 infection: What do we know and what don't we know? Infection Control & Hospital Epidemiology. 2021:1-7. [view at publisher] [DOI] [Google Scholar]
25. Shamszadeh S, Parhizkar A, Mardani M, Asgary S. Dental Considerations After the Outbreak of 2019 Novel Coronavirus Disease: A Review of Literature. Arch Clin Infect Dis. 2020;15(2):e103257. [view at publisher] [DOI] [Google Scholar]
26. Guidelines for the Prevention D, and Treatment, of Novel Coronavirus-induced Pneumonia Tte, http://www.nhc.gov.cn/yzygj/s7653p/202002/d4b89533, 7e19445f8d728fcaf1e3e13a/files/ab6bec7f93e64e7f99, 8d802991203cd6.pdf (accessed February 18 i, Chinese).
27. National Health Commission. General Office of National Health Commission. A Notice on the Issuance of Technical Guidelines on the Prevention and Control of Novel Coronavirus Pneumonia in Medical Institutions (First edition). Available at: http://www.nhc.gov.cn/yzygj/s7659/202001/b91fdab7c304431eb082d67847d27e14.shtml. Accessed January 22, 2020.
28. Ather A, Patel B, Ruparel NB, Diogenes A, Hargreaves KM. Coronavirus Disease 19 (COVID-19): Implications for Clinical Dental Care. J Endod. 2020;46(5):584-95. [view at publisher] [DOI] [Google Scholar]
29. Bentivegna E, Sentimentale A, Luciani M, Speranza M, Guerritore L, Martelletti P. New IgM seroconversion and positive RT‐PCR test after exposure to the virus in recovered COVID‐19 patient. Journal of Medical Virology. 2020;93. [view at publisher] [DOI] [Google Scholar]
30. Liu G, Rusling J. COVID-19 Antibody Tests and Their Limitations. ACS Sensors. 2021. [view at publisher] [DOI] [Google Scholar]
31. Stanley J, Sethuraman N, Ryo A. Interpreting Diagnostic Tests for SARS-CoV-2. JAMA. 2020;323. [view at publisher] [DOI] [Google Scholar]
32. Lan L, Xu D, Ye G, Xia C, Wang S, Li Y, et al. Positive RT-PCR Test Results in Patients Recovered from COVID-19. JAMA. 2020;323. [view at publisher] [DOI] [Google Scholar]
33. Long Q-X, Liu B-Z, Deng H-J, Wu G-C, Deng K, Chen Y-K, et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nature Medicine. 2020;26(6):845-8. [view at publisher] [DOI] [Google Scholar]
34. Gonçalves J, Sousa RL, Jacinto MJ, Silva DA, Paula F, Sousa R, et al. Evaluating SARS-CoV-2 Seroconversion Following Relieve of Confinement Measures. Frontiers in Medicine. 2020;7(971). [view at publisher] [DOI] [Google Scholar]
35. Sawhney A, Venugopal S, Babu GR, Garg A, Mathew M, Yadav M, et al. Aerosols how dangerous they are in clinical practice. J Clin Diagn Res. 2015;9(4):Zc52-7. [view at publisher] [DOI] [Google Scholar]
36. Kobza J, Pastuszka JS, Bragoszewska E. Do exposures to aerosols pose a risk to dental professionals? Occup Med (Lond). 2018;68(7):454-8. [view at publisher] [DOI] [Google Scholar]
37. Yamada H, Ishihama K, Yasuda K, Hasumi-Nakayama Y, Shimoji S, Furusawa K. Aerial dispersal of blood-contaminated aerosols during dental procedures. Quintessence Int. 2011;42(5):399-405. [view at publisher] [Google Scholar]
38. Belser JA, Gustin KM, Katz JM, Maines TR, Tumpey TM. Influenza virus infectivity and virulence following ocular-only aerosol inoculation of ferrets. J Virol. 2014;88(17):9647-54. [view at publisher] [DOI] [Google Scholar]
39. Carrouel F, Conte MP, Fisher J, Goncalves LS, Dussart C, Llodra JC, et al. COVID-19: A Recommendation to Examine the Effect of Mouthrinses with beta-Cyclodextrin Combined with Citrox in Preventing Infection and Progression. J Clin Med. 2020;9(4). [view at publisher] [DOI] [Google Scholar]
40. Jin Y-H, Cai L, Cheng Z-S, Cheng H, Deng T, Fan Y-P, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Military Medical Research. 2020;7(1):4. [view at publisher] [DOI] [Google Scholar]
41. Li ZY, Meng LY. [The prevention and control of a new coronavirus infection in department of stomatology]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2020;55(0):E001. [view at publisher] [Google Scholar]
42. Carrouel F, Gonçalves LS, Conte MP, Campus G, Fisher J, Fraticelli L, et al. Antiviral Activity of Reagents in Mouth Rinses against SARS-CoV-2. J Dent Res. 2021;100(2):124-32. [DOI]
43. Kathuria V, Ankola AV, Hebbal M, Mocherla M. Carisolv- an innovative method of caries removal. J Clin Diagn Res. 2013;7(12):3111-5. [view at publisher] [Google Scholar]
44. Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. New England Journal of Medicine. 2020;382(16):1564-7. [view at publisher] [DOI] [Google Scholar]
45. Siegel JD, Rhinehart E, Jackson M, Chiarello L. 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Health Care Settings. Am J Infect Control. 2007;35(10 Suppl 2):S65-164. [DOI] [Google Scholar]
46. Merethe C. Lind MSHKDBVAWV, M.Sc.; Petri Kalliomäki, M.Sc.; Trond Thorgeir Harsem, M.Sc., Member ASHRAE. Designing Simplified Airborne Infection Isolation Rooms to Reduce Infection Rate in Future Pandemics. ASHRAE Transactions papers2020. p. 280-7. [view at publisher] [Google Scholar]
47. Sparks T, Chase G. Section 3 - Air and Gas Filtration. In: Sparks T, Chase G, editors. Filters and Filtration Handbook (Sixth Edition). Oxford: Butterworth-Heinemann; 2016. p. 117-98. [view at publisher] [DOI] [Google Scholar]
48. Jensen PA, Lambert LA, Iademarco MF, Ridzon R. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep. 2005;54(Rr-17):1-141. [view at publisher] [Google Scholar]
49. Panov V, Borisova-Papancheva T. Application of ultraviolet light (UV) in dental medicdine. Journal of Medical and Dental Practice. 2015;2:194-200. [DOI] [Google Scholar]
50. Kowalski W, Walsh T, Petraitis V. 2020 COVID-19 Coronavirus Ultraviolet Susceptibility2020. [Google Scholar]
51. Arguelles P. Estimating UV-C Sterilization Dosage for COVID-19 Pandemic Mitigation Efforts2020. [Google Scholar]
52. Hemalatha R GD. Disinfection of Dental Impression- A Current Overview. Int J Pharm Sci Res. 2016;8(7):661-4. [view at publisher] [Google Scholar]
53. Mushtaq MA, Khan M. An Overview of Dental Impression Disinfection Techniques-A Literature Review. 2019;27. [DOI] [Google Scholar]
54. Lepe X, Johnson GH, Berg JC. Surface characteristics of polyether and addition silicone impression materials after long-term disinfection. J Prosthet Dent. 1995;74(2):181-6. [view at publisher] [DOI] [Google Scholar]
55. Van Noort R. Impression materials in: Introduction to Dental Materials. 3rd ed: Mosby Elsevier; 2007.
56. Doddamani S, Patil RA, Gangadhar SA. Efficacy of various spray disinfectants on irreversible hydrocolloid impression materials: an in vitro study. Indian J Dent Res. 2011;22(6):764-9. [view at publisher] [DOI] [Google Scholar]
57. Coronavirus infectious waste management. British Dental Journal. 2020;228(10):802 [DOI]
58. Alanisamy Pasupathi SS, Babu Shankar Ponnusha , Athimoolam Ambika. Biomedical waste management for health care industry. Int J Biol Med Res. 2011;2(1):472 - 86 [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |